
The use of gadolinium contrast with MRI should be limited it may be used as a contrast agent in a pregnant woman only if it significantly improves diagnostic performance and is expected to improve fetal or maternal outcome.īreastfeeding should not be interrupted after gadolinium administration. If these techniques are necessary in addition to ultrasonography or MRI or are more readily available for the diagnosis in question, they should not be withheld from a pregnant patient. With few exceptions, radiation exposure through radiography, computed tomography (CT) scan, or nuclear medicine imaging techniques is at a dose much lower than the exposure associated with fetal harm. Ultrasonography and magnetic resonance imaging (MRI) are not associated with risk and are the imaging techniques of choice for the pregnant patient, but they should be used prudently and only when use is expected to answer a relevant clinical question or otherwise provide medical benefit to the patient. The American College of Obstetricians and Gynecologists’ Committee on Obstetric Practice makes the following recommendations regarding diagnostic imaging procedures during pregnancy and lactation: Breastfeeding should not be interrupted after gadolinium administration. If these techniques are necessary in addition to ultrasonography or magnetic resonance imaging or are more readily available for the diagnosis in question, they should not be withheld from a pregnant patient. With few exceptions, radiation exposure through radiography, computed tomography scan, or nuclear medicine imaging techniques is at a dose much lower than the exposure associated with fetal harm. Ultrasonography and magnetic resonance imaging are not associated with risk and are the imaging techniques of choice for the pregnant patient, but they should be used prudently and only when use is expected to answer a relevant clinical question or otherwise provide medical benefit to the patient. However, confusion about the safety of these modalities for pregnant and lactating women and their infants often results in unnecessary avoidance of useful diagnostic tests or the unnecessary interruption of breastfeeding.

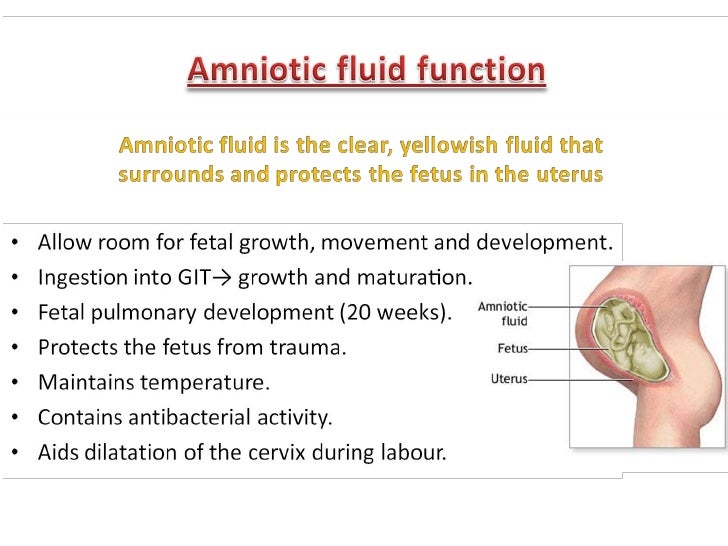
The test is best performed between 15-16 weeks.ABSTRACT: Imaging studies are important adjuncts in the diagnostic evaluation of acute and chronic conditions. The foetus grows in the uterus, or womb, inside a bag called the “amniotic sac” surrounded by amniotic fluid.Īmniotic fluid is made by the placenta (the organ that develops inside the uterus to supply food and oxygen, through the umbilical cord, to the foetus) but contains cells and proteins from the foetus which can be tested for the sex of the baby and chromosomal abnormalities such as Down syndrome.Ībout 130 mL of fluid surrounds the foetus at 16 weeks and only 20 mL are removed which is naturally replaced by the placenta within 24 hours. who are anxious for other reasons about the possibility of their foetus having a chromosomal abnormality.Īmniocentesis is a procedure where a needle is inserted into the abdomen to obtain a small amount of amniotic fluid.with a high risk as a result of first trimester screening (see nuchal translucency scan).with a personal or family history of a chromosomal abnormality or a partner with such a personal or family history.who have had an abnormality in their foetus or unborn baby identified on an ultrasound scan.

18-20 week screening pregnancy ultrasound.


 0 kommentar(er)
0 kommentar(er)
